mrabbi [at] illinois [dot] edu
CV | Google Scholar |
Research statement
Mobile health
Mobile sensing of health behavior
Personalized intervention
Just-in-time intervention
Applied ML and RL
Human-centered AI
Teaching
CS-598: AI applied to behavioral health
Want to join our lab?
Please see this FAQ page.
Assistant Research Professor
Siebel School of Computing and Data Science
University of Illinois, Urbana-Champaign
My lab focuses on mobile health with the specific aim to provide the right intervention
at the right time for the right person. We use
off-the-shelf mobile and wearable devices to understand health behaviors and provide
personalized, just-in-time interventions tailored to users' needs, daily routines, and
their environments.
While my research include predicting health and well-being from mobile data
(e.g., predicting stress and mental health from phone sensor data; Rabbi 2011; Lu et al. 2012),
I am highly interested in using these predictions to close the loop by
providing feedback and insights to patients and providers. To this end,
my lab works in the following three broad areas.
-
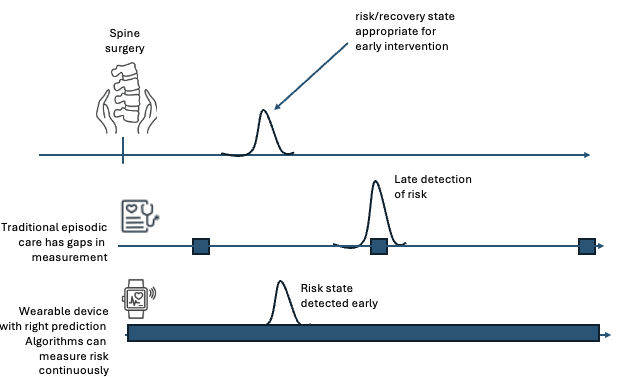
Sensing clinically actionable health risk: Early detection of health
risks can improve health outcomes and reduce costs. We utilize machine learning
on continuously sensed data to detect risks early. See an example below, our wok on spine
surgery recovery project below where we are fine-tuning a custom-built motion
foundation model to early predict recovery states after surgery.
.
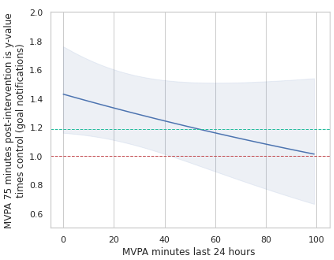
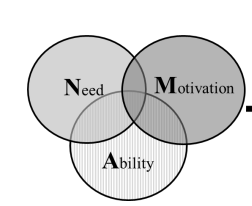
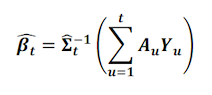
- Personalized and just-in-time intervention :
Mobile and wearable devices offer a unique opportunity to deliver interventions
and provide support when people are not in the clinic. To this end, we use
behavioral science, sequential experimentation, and reinforcement learning
to identify personalized and contextual interventions. Our data-driven
approach makes interventions more timely and better aligned with a user’s
lifestyle, needs, and goals. A key challenge in this area is managing
high-dimensional contexts and the long-term, noisy effects of interventions.
-
Integration with healthcare systems: In this line of work,
we directly partner with providers to build solutions for patients in need.
We create actionable, data-driven insights that are
low-burden for providers to use. For example, in our work on shared
medical appointments, we are developing low-burden insights from wearable
devices and electronic health records for providers serving patients in
rural Illinois.
News
- May, 2025: I joined University of Illinois, Urbana-Champaign as an assistant research professor
- Aug, 2024: Invited talk at Computer Science Seminar at University of Illinois, Urbana-Champaign
- Oct, 2023: Invited talk at Link Lab research day at University of Virginia
- Nov, 2019: Invited talk at HCII seminar at CMU
- Oct, 2019: Invited talk at mHealth Research Affinity Group at Children's Hospital of Philadelphia
- Oct, 2019: Invited talk at HIV working group. at Harvard Biostatistics Dept[slides]
- Sep, 2019: Invited talk at School of Biomedical Informatics at University of Texas Health Science Center
- June, 2019: Invited talk at Turi at Apple Inc., Seattle, WA [slides]
Projects
Leveraging AI to reduce clinician burden and improve social support in group-medical visits
Group medical visits are an innovative care delivery mechanism where multiple
providers see multiple patients at the same time. Such group visits are
specially useful for rural healthcare where patients and providers live far from
the clinic; i.e., setting up 1-on-1 visits with patients and
providers are difficult.
This project aims to reduce provider burden and improve social support
for patients. To strengthen social support, we analyze sleep behaviors
captured by wearable devices to identify actionable insights. We then match
patients for whom similar actionable insights apply, under the idea that
people are more likely to act on behaviors of similar users (social proof).
To reduce provider burden, we learn patient embeddings from electronic medical
records to detect vulnerable patients early and group similar patients together
for group medical visits.
Early prediction of spine surgery recovery states using foundation models
This project evaluates the feasibility of using a foundation model
to predict actionable states
for patients undergoing spine surgery. These actionable states are gold-standard
movement and gait metrics
that clinicians rely on to evaluate recovery progress after surgery. Currently,
such assessments occur
only during periodic clinic visits, which may miss optimal intervention times.
Our goal is to use wearable
technology to predict these metrics early and continuously, enabling clinicians
to intervene effectively and
improve patient outcomes, such as reducing readmission rates.
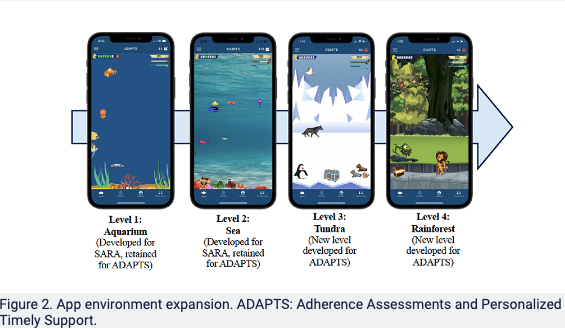
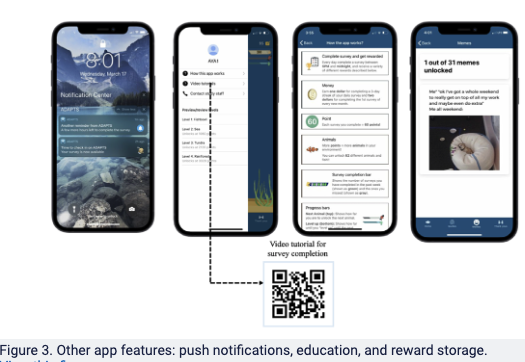
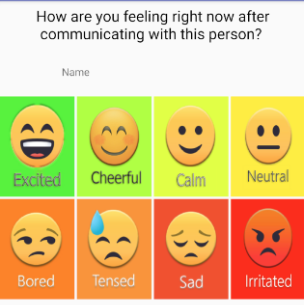
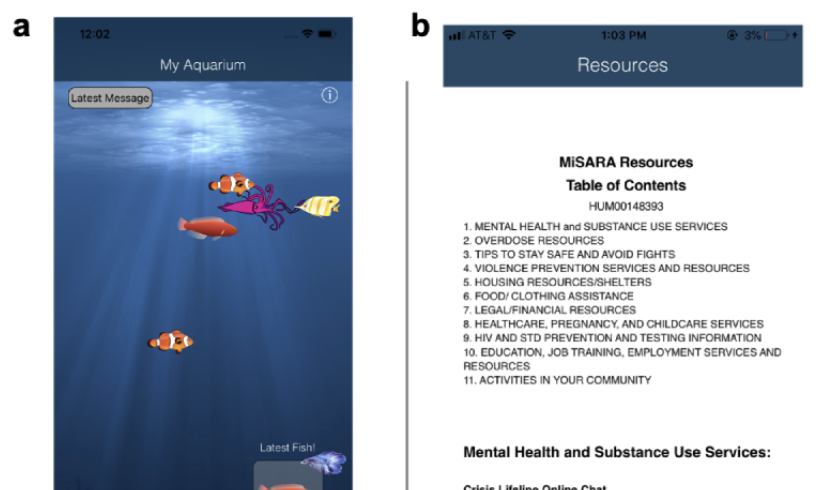
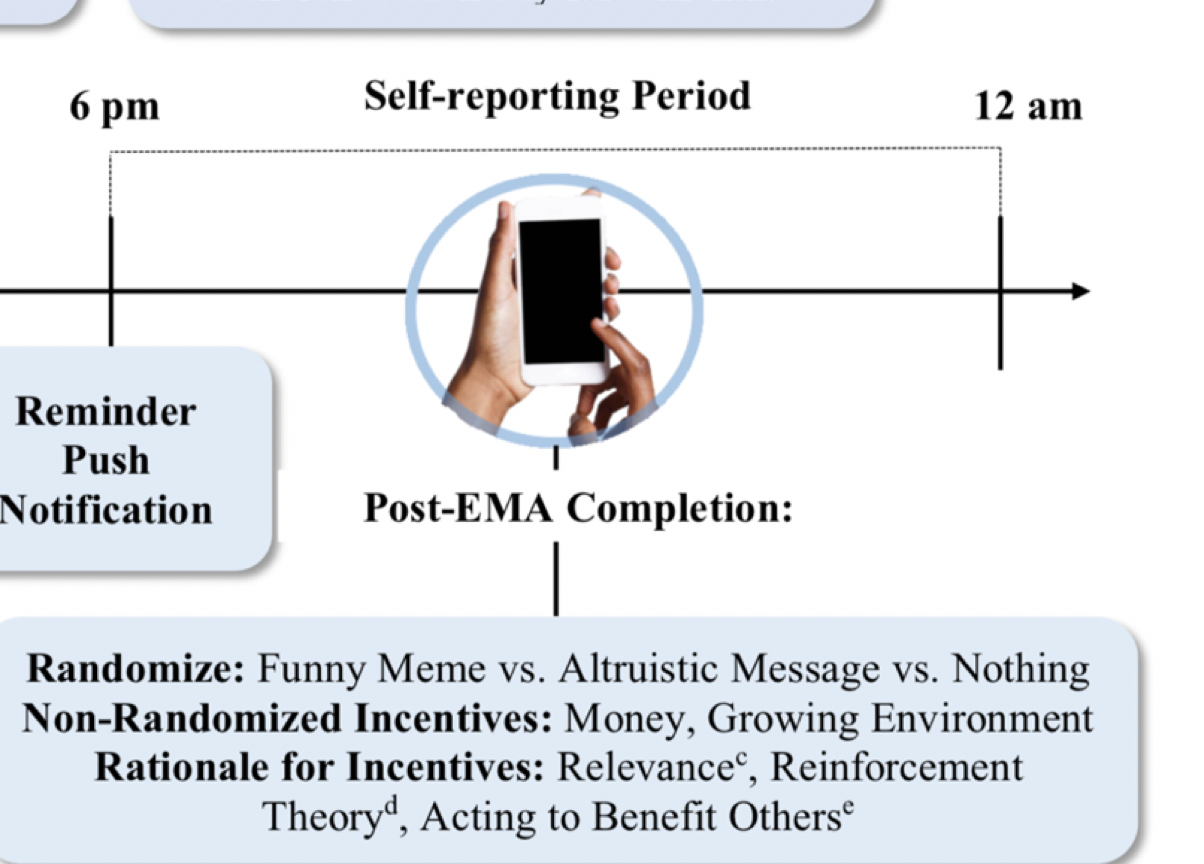
SARA: Just-in-time intervention for improving engagement
Self-report adherence of mobile health apps are generally low.
SARA (Substance Abuse Research Assistant) is the
first just-in-time intervention to
increase self-report adherence with timely rewards or inspirational messages.
Initial deployments
of SARA target adolescents and younger adults at high risk of substance abuse.
Related papers: study protocol, results from micro-randomized trial, just-in-time intervention to improve substance use . See below the ADAPTS project that uses SARA for yonger adults with lukemia. A recent R01 grant is founded that will SARA on sickle cell disease patients.
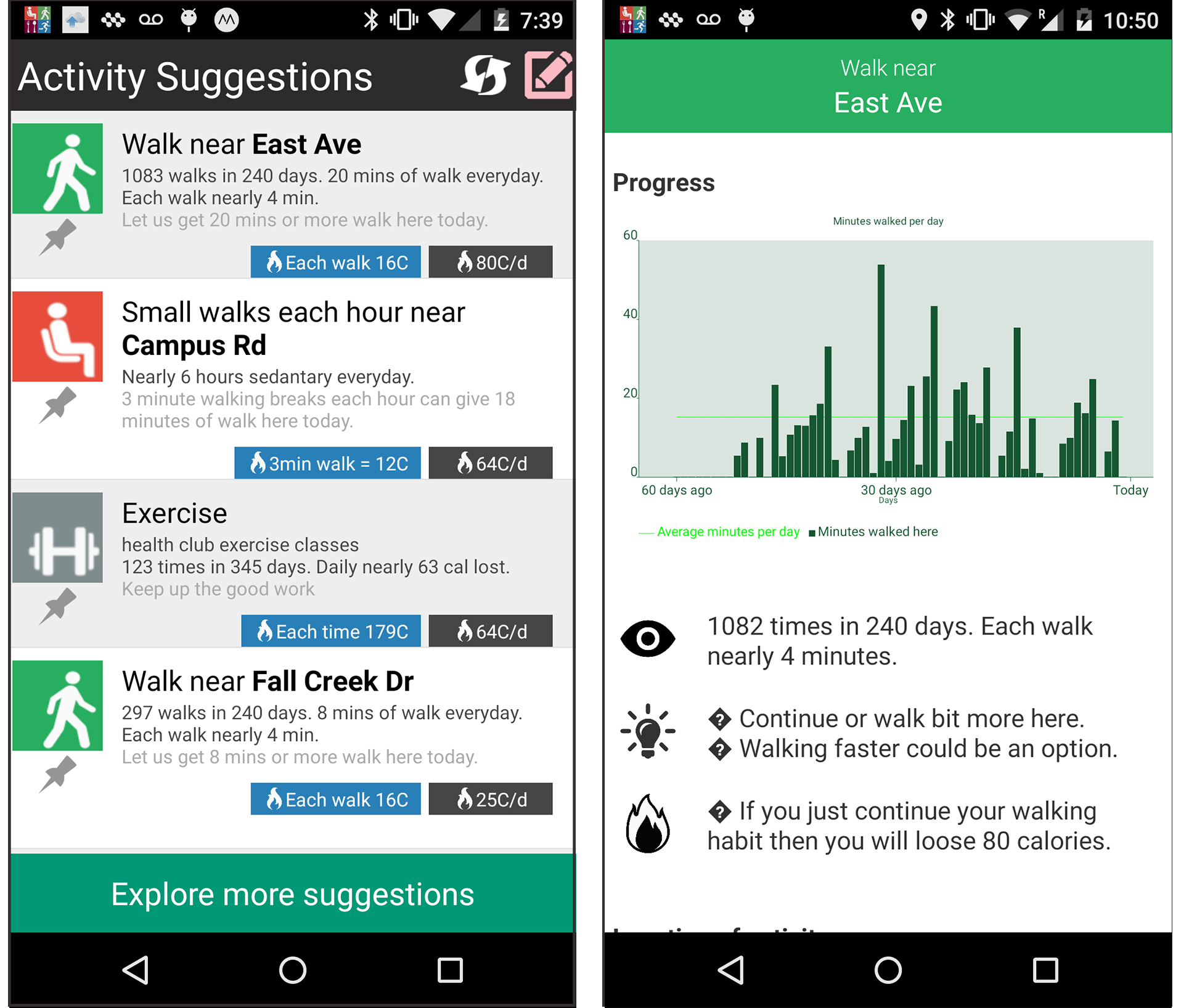
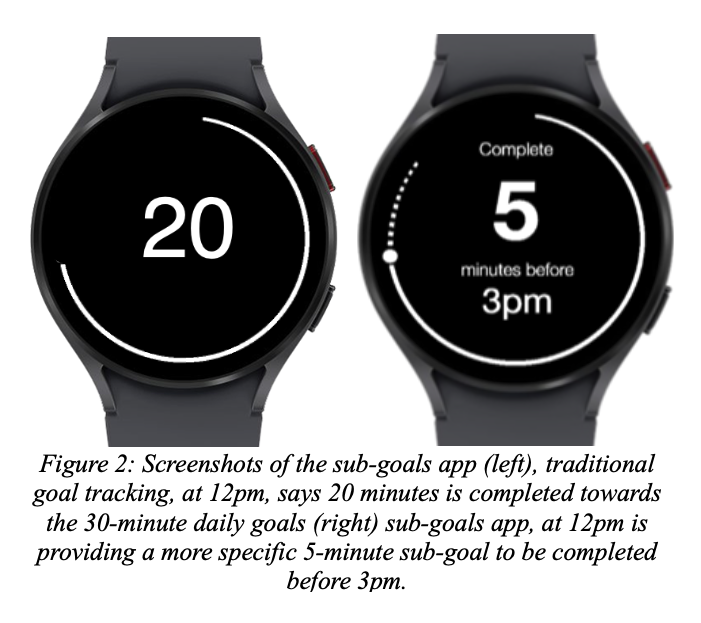
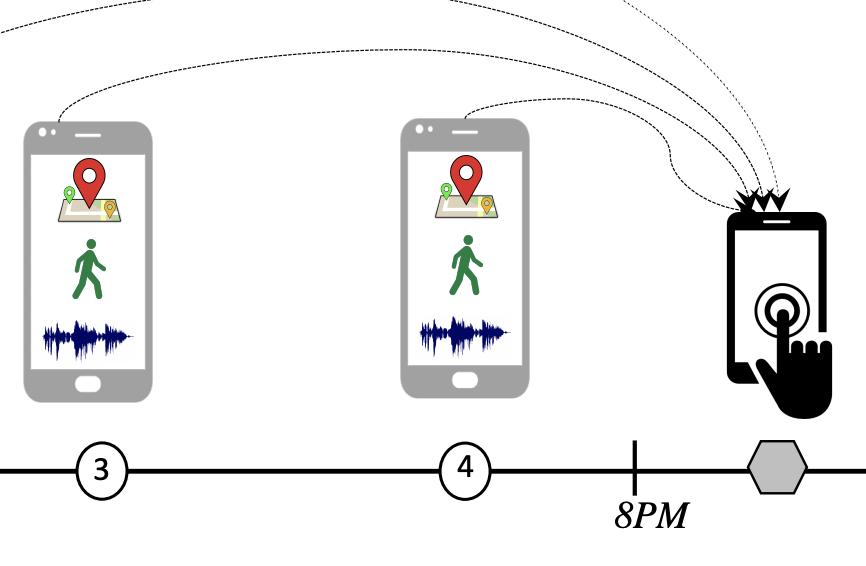
Sub-goal app
The sub-goals app divides a daily physical activity goal into a personalized subgoal plan
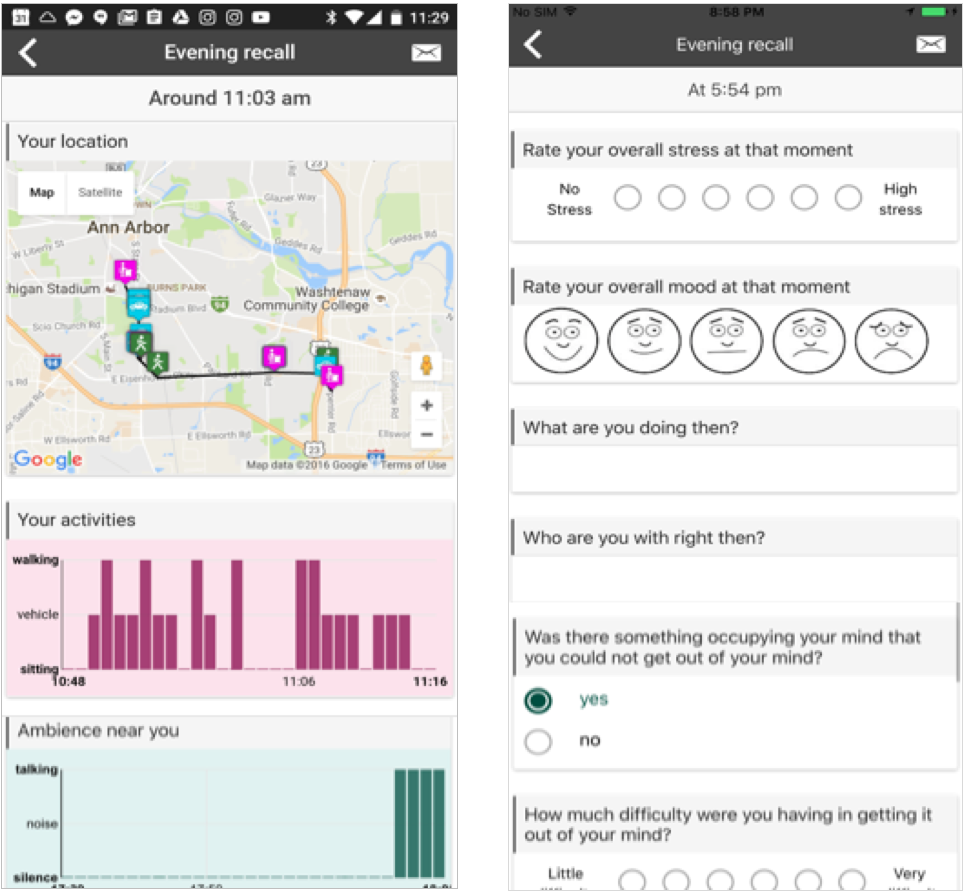
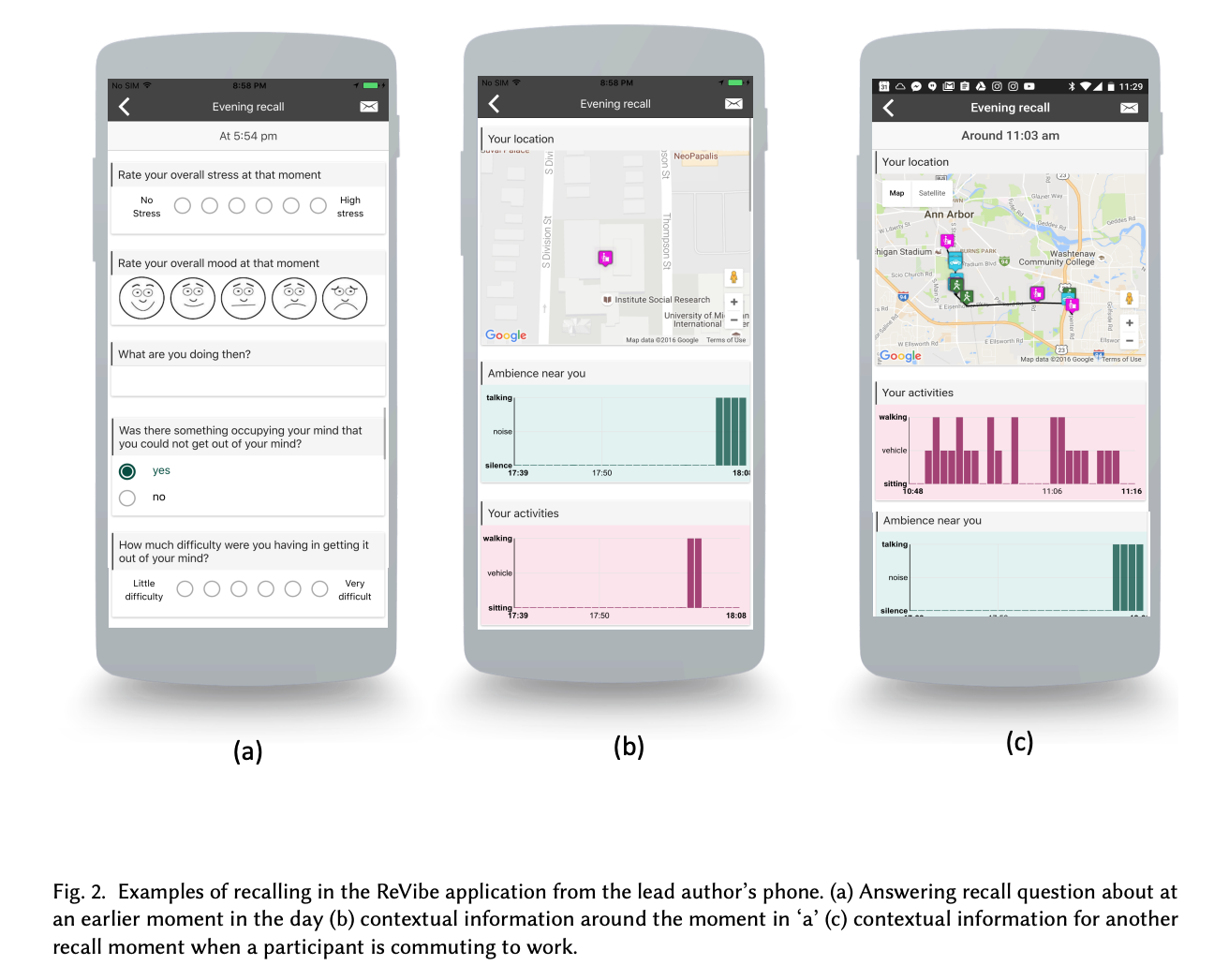
ReVibe
ReVibe uses context-assisted recall in the evening instead of in the moment Ecological Momentary Assessments (EMA) to increase self-report adherance
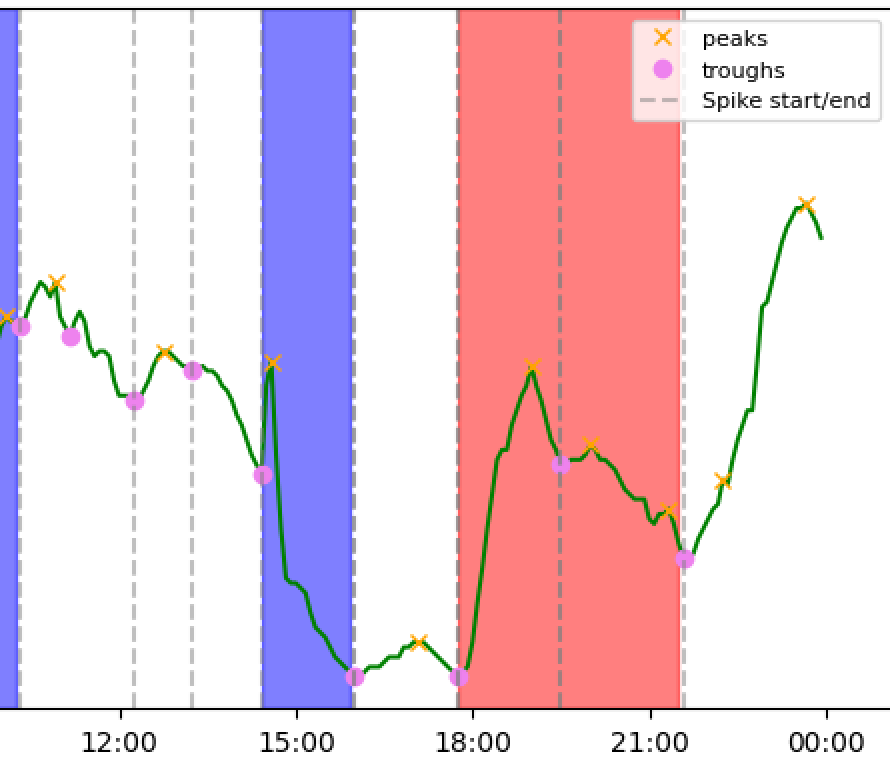
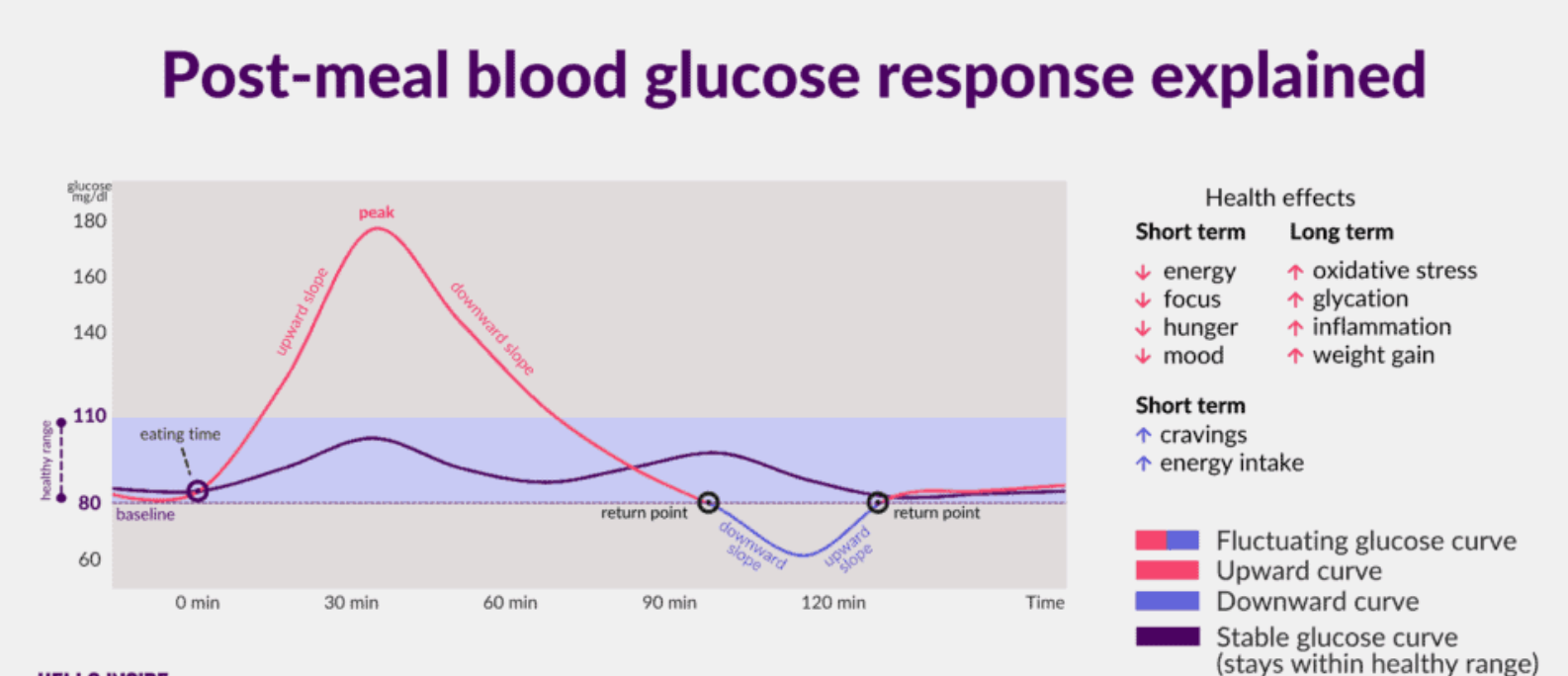
Glucose spike control
Repeated glucose spikes can develop type-2 diabetes (T2D) or worsen existing T2D. This project creates a just-in-time walking intervention to curb glucose spikes before they reach harmful levels.
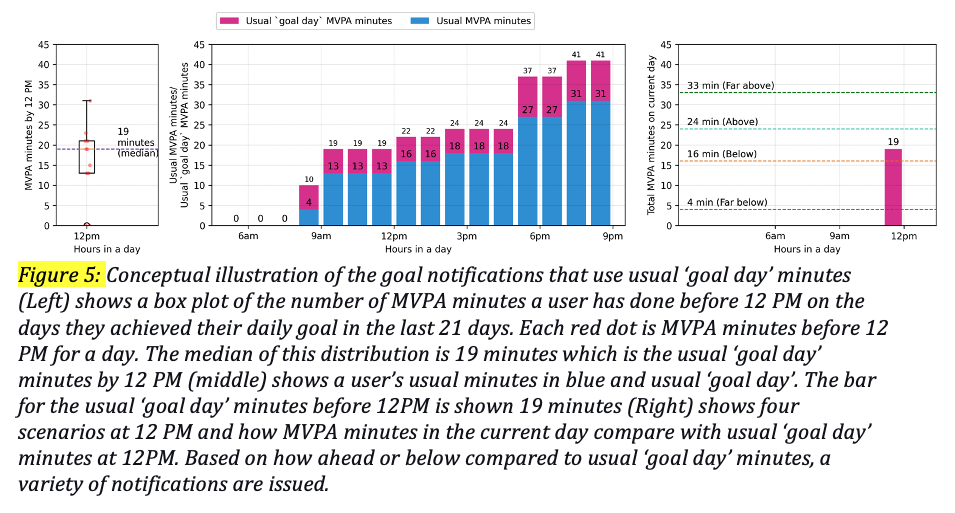
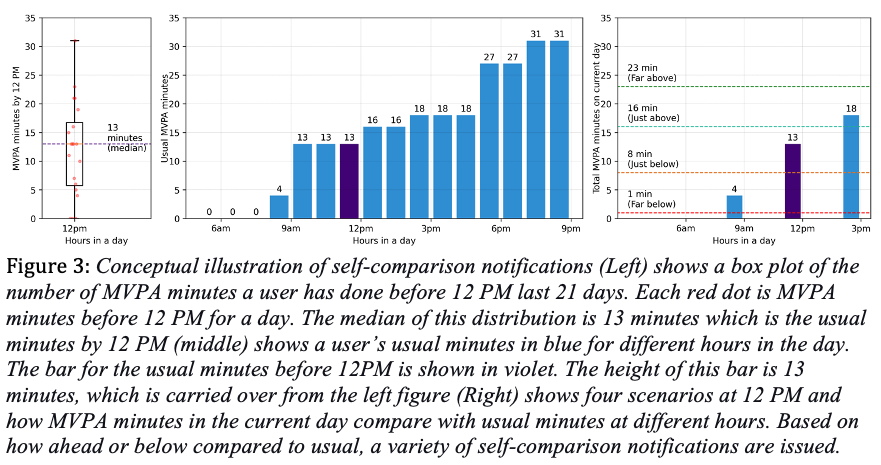
pi2 messages
pi2 messages are pesonalized just-in-time physical activity messages that use data-driven insights of a user's usual activity levels and progress towards their goals.
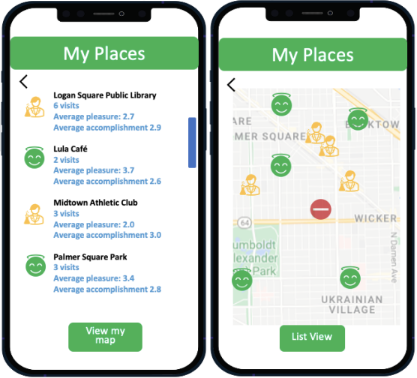
Mobilyze
Mobilyze focueses on people with depression. It uses gamification and sensing to encourage visiting places a user is familiar with. Broadening these visited locations can improve depressive symptoms.
BeWell
BeWell app provides multi-dimensional feedback on daily physical activity, sleep and socialization.
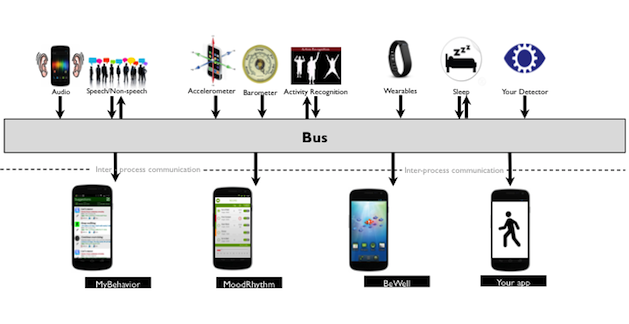
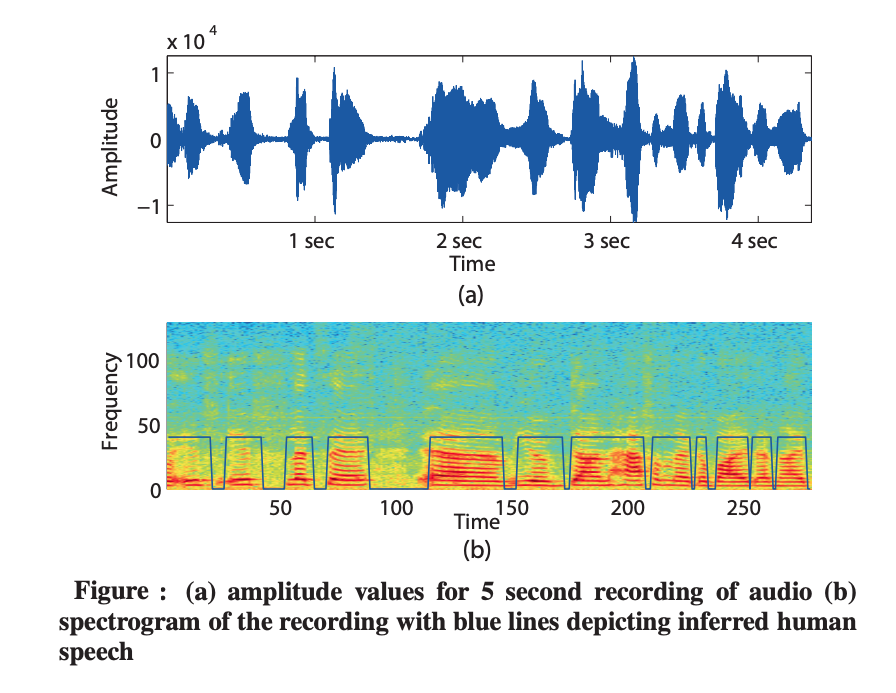
Mental health sensing
This 2011 project on passive sensing of mental health using audio and accelerometer data, kickstarted the research in mental health sensing.
PUBLICATIONS
Citation count: 3830 (updated August 25, 2025) Google scholar contains a more up-to-date publication list.Refereed conference and journal publications
-
28.
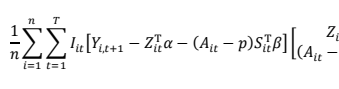 Tianchen Qian, Ashley E Walton, Linda M Collins, Predrag Klasnja, Stephanie T Lanza, Inbal Nahum-Shani, Mashfiqui Rabbi, Michael A Russell, Maureen A Walton, Hyesun Yoo, Susan A Murphy The microrandomized trial for developing digital interventions: Experimental design and data analysis considerations. Psychological methods. 2022 [pdf]
Tianchen Qian, Ashley E Walton, Linda M Collins, Predrag Klasnja, Stephanie T Lanza, Inbal Nahum-Shani, Mashfiqui Rabbi, Michael A Russell, Maureen A Walton, Hyesun Yoo, Susan A Murphy The microrandomized trial for developing digital interventions: Experimental design and data analysis considerations. Psychological methods. 2022 [pdf]
-
27.
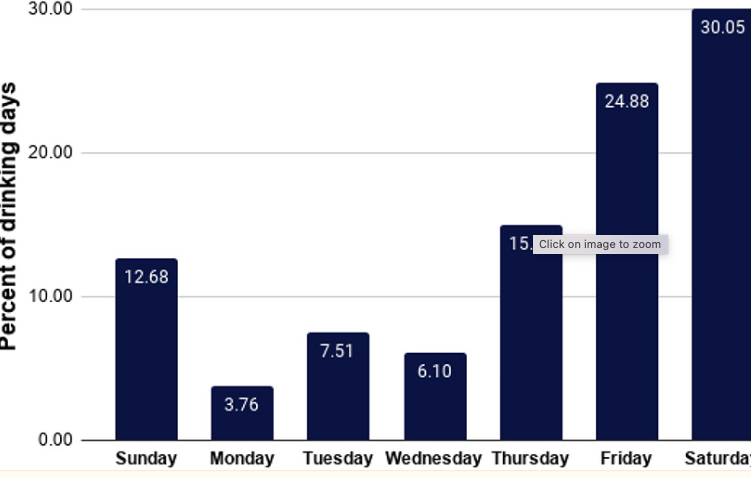 Lara N Coughlin, Inbal Nahum-Shani, Erin E Bonar, Meredith L Philyaw-Kotov, Mashfiqui Rabbi, Predrag Klasnja, Maureen A Walton Toward a just-in-time adaptive intervention to reduce emerging adult alcohol use: testing approaches for identifying when to intervene. Substance use & misuse 56 (14), 2115-2125 [pdf]
Lara N Coughlin, Inbal Nahum-Shani, Erin E Bonar, Meredith L Philyaw-Kotov, Mashfiqui Rabbi, Predrag Klasnja, Maureen A Walton Toward a just-in-time adaptive intervention to reduce emerging adult alcohol use: testing approaches for identifying when to intervene. Substance use & misuse 56 (14), 2115-2125 [pdf]
-
26.
 Inbal Nahum-Shani, Mashfiqui Rabbi, Jamie Yap, Meredith L Philyaw-Kotov, Predrag Klasnja, Erin E Bonar, Rebecca M Cunningham, Susan A Murphy, Maureen A Walton Translating strategies for promoting engagement in mobile health: A proof-of-concept microrandomized trial. Health Psychology, 40(12), 974–987 [pdf]
Inbal Nahum-Shani, Mashfiqui Rabbi, Jamie Yap, Meredith L Philyaw-Kotov, Predrag Klasnja, Erin E Bonar, Rebecca M Cunningham, Susan A Murphy, Maureen A Walton Translating strategies for promoting engagement in mobile health: A proof-of-concept microrandomized trial. Health Psychology, 40(12), 974–987 [pdf]
-
25.
 Ananya Bhattacharjee, SM Taiabul Haque, Md Abdul Hady, SM Raihanul Alam, Mashfiqui Rabbi, Muhammad Ashad Kabir, Syed Ishtiaque Ahmed Understanding the social determinants of mental health of undergraduate students in Bangladesh: Interview study JMIR Formative Research 2021;5(11):e27114 [pdf]
Ananya Bhattacharjee, SM Taiabul Haque, Md Abdul Hady, SM Raihanul Alam, Mashfiqui Rabbi, Muhammad Ashad Kabir, Syed Ishtiaque Ahmed Understanding the social determinants of mental health of undergraduate students in Bangladesh: Interview study JMIR Formative Research 2021;5(11):e27114 [pdf]
-
24.
 Alexandra M Psihogios, Mashfiqui Rabbi, Annisa Ahmed, Elise R McKelvey, Yimei Li, Jean-Philippe Laurenceau, Stephen P Hunger, Linda Fleisher, Ahna LH Pai, Lisa A Schwartz, Susan A Murphy, Lamia P Barakat Understanding adolescent and young adult 6-mercaptopurine adherence and mHealth engagement during cancer treatment: protocol for ecological momentary assessment JMIR Research Protocol 2021;10(10):e32789 [pdf]
Alexandra M Psihogios, Mashfiqui Rabbi, Annisa Ahmed, Elise R McKelvey, Yimei Li, Jean-Philippe Laurenceau, Stephen P Hunger, Linda Fleisher, Ahna LH Pai, Lisa A Schwartz, Susan A Murphy, Lamia P Barakat Understanding adolescent and young adult 6-mercaptopurine adherence and mHealth engagement during cancer treatment: protocol for ecological momentary assessment JMIR Research Protocol 2021;10(10):e32789 [pdf]
-
23.
 Lara N Coughlin, Inbal Nahum-Shani, Meredith L Philyaw-Kotov, Erin E Bonar, Mashfiqui Rabbi, Predrag Klasnja, Susan Murphy, Maureen A Walton Developing an Adaptive Mobile Intervention to Address Risky Substance Use Among Adolescents and Emerging Adults: sability Study JMIR Mhealth Uhealth 2021;9(1):e24424 [Impact factor 4.3] [pdf]
Lara N Coughlin, Inbal Nahum-Shani, Meredith L Philyaw-Kotov, Erin E Bonar, Mashfiqui Rabbi, Predrag Klasnja, Susan Murphy, Maureen A Walton Developing an Adaptive Mobile Intervention to Address Risky Substance Use Among Adolescents and Emerging Adults: sability Study JMIR Mhealth Uhealth 2021;9(1):e24424 [Impact factor 4.3] [pdf]
-
22.
 Shuang Li, Alexandra M Psihogios, Elise R McKelvey, Annisa Ahmed, Mashfiqui Rabbi, Susan Murphy Microrandomized trials for promoting engagement in mobile health data collection: Adolescent/young adult oral chemotherapy adherence as an example Current Opinion in Systems Biology, (2020), Elsevier
Shuang Li, Alexandra M Psihogios, Elise R McKelvey, Annisa Ahmed, Mashfiqui Rabbi, Susan Murphy Microrandomized trials for promoting engagement in mobile health data collection: Adolescent/young adult oral chemotherapy adherence as an example Current Opinion in Systems Biology, (2020), Elsevier
-
21.
 Mashfiqui Rabbi, Katherine Li, H Yanna Yan, Kelly Hall, Predrag Klasnja, Susan Murphy ReVibe: A Context-assisted Evening Recall Approach to Improve Self-report Adherence Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies, 3, 4, 1--27 (2019), ACM New York, NY, USA:[pdf]
Mashfiqui Rabbi, Katherine Li, H Yanna Yan, Kelly Hall, Predrag Klasnja, Susan Murphy ReVibe: A Context-assisted Evening Recall Approach to Improve Self-report Adherence Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies, 3, 4, 1--27 (2019), ACM New York, NY, USA:[pdf]
-
20.
 Marianne Menictas*, Mashfiqui Rabbi*, Predrag Klasnja, Susan Murphy Artificial intelligence decision-making in mobile health The Biochemist, 41, 5, 20--24 (2019):[pdf] * authors equally contributed
Marianne Menictas*, Mashfiqui Rabbi*, Predrag Klasnja, Susan Murphy Artificial intelligence decision-making in mobile health The Biochemist, 41, 5, 20--24 (2019):[pdf] * authors equally contributed
-
19.
 Mashfiqui Rabbi, Predrag Klasnja, Tanzeem Choudhury, Ambuj Tewari, and Susan Murphy. Optimizing mHealth Interventions with a Bandit Mobile Sensing and Digital Phenotyping: New Developments in Psychoinformatics, Springer: Berlin [preprint]
Mashfiqui Rabbi, Predrag Klasnja, Tanzeem Choudhury, Ambuj Tewari, and Susan Murphy. Optimizing mHealth Interventions with a Bandit Mobile Sensing and Digital Phenotyping: New Developments in Psychoinformatics, Springer: Berlin [preprint]
-
18.
 Mashfiqui Rabbi, Min SH Aung, Geri Gay, M. Cary Reid, and Tanzeem Choudhury. Feasibility and Acceptability of Mobile Phone–Based Auto-Personalized Physical Activity Recommendations for Chronic Pain Self-Management: Pilot Study on Adults Journal of Medical Internet Research 20, no. 10 (2018): e10147. [Impact factor 4.6] [pdf]
Mashfiqui Rabbi, Min SH Aung, Geri Gay, M. Cary Reid, and Tanzeem Choudhury. Feasibility and Acceptability of Mobile Phone–Based Auto-Personalized Physical Activity Recommendations for Chronic Pain Self-Management: Pilot Study on Adults Journal of Medical Internet Research 20, no. 10 (2018): e10147. [Impact factor 4.6] [pdf]
-
17.
 Mashfiqui Rabbi, Meredith Philyaw Kotov, Rebecca Cunningham, Erin E. Bonar, Inbal Nahum-Shani, Predrag Klasnja, Maureen Walton, and Susan Murphy Toward Increasing Engagement in Substance Use Data Collection: Development of the Substance Abuse Research Assistant App and Protocol for a Microrandomized Trial Using Adolescents and Emerging Adults JMIR Research Protocols 7, no. 7 (2018): e166. [pdf]
Mashfiqui Rabbi, Meredith Philyaw Kotov, Rebecca Cunningham, Erin E. Bonar, Inbal Nahum-Shani, Predrag Klasnja, Maureen Walton, and Susan Murphy Toward Increasing Engagement in Substance Use Data Collection: Development of the Substance Abuse Research Assistant App and Protocol for a Microrandomized Trial Using Adolescents and Emerging Adults JMIR Research Protocols 7, no. 7 (2018): e166. [pdf]
-
16.
 Mashfiqui Rabbi, Min Hane Aung, and Tanzeem Choudhury. Towards health recommendation systems: an approach for providing automated personalized health feedback from mobile data. In: Rehg J., Murphy S., Kumar S. (eds) Mobile Health. Springer, Cham, 2017 [pdf]
Mashfiqui Rabbi, Min Hane Aung, and Tanzeem Choudhury. Towards health recommendation systems: an approach for providing automated personalized health feedback from mobile data. In: Rehg J., Murphy S., Kumar S. (eds) Mobile Health. Springer, Cham, 2017 [pdf]
-
15.
 Eun Kyoung Choe, Saeed Abdullah, Mashfiqui Rabbi, Edison Thomaz, Daniel A. Epstein, Felicia Cordeiro, Matthew Kay et al. Semi-automated tracking: A balanced approach for self-monitoring applications. IEEE Pervasive Computing 16, no. 1 (2017): 74-84.[pdf]
Eun Kyoung Choe, Saeed Abdullah, Mashfiqui Rabbi, Edison Thomaz, Daniel A. Epstein, Felicia Cordeiro, Matthew Kay et al. Semi-automated tracking: A balanced approach for self-monitoring applications. IEEE Pervasive Computing 16, no. 1 (2017): 74-84.[pdf]
-
14.
 Aung, Min S. Hane, Faisal Alquaddoomi, Cheng-Kang Hsieh, Mashfiqui Rabbi, Longqi Yang, John P. Pollak, Deborah Estrin, and Tanzeem Choudhury. Leveraging multi-modal sensing for mobile health: a case review in chronic pain. IEEE Journal of Selected Topics in Signal Processing 10, no. 5 (2016): 962-974.[ pdf]
Aung, Min S. Hane, Faisal Alquaddoomi, Cheng-Kang Hsieh, Mashfiqui Rabbi, Longqi Yang, John P. Pollak, Deborah Estrin, and Tanzeem Choudhury. Leveraging multi-modal sensing for mobile health: a case review in chronic pain. IEEE Journal of Selected Topics in Signal Processing 10, no. 5 (2016): 962-974.[ pdf]
-
13.
 Mashfiqui Rabbi, Jean Costa, Fabian Okeke, Max Schachere, Mi Zhang, and Tanzeem Choudhury. An Intelligent Crowd-worker Selection Approach for Reliable Content Labeling of Food Images. The Proceedings of Wireless Health 2015 [pdf].
Mashfiqui Rabbi, Jean Costa, Fabian Okeke, Max Schachere, Mi Zhang, and Tanzeem Choudhury. An Intelligent Crowd-worker Selection Approach for Reliable Content Labeling of Food Images. The Proceedings of Wireless Health 2015 [pdf].
-
12.
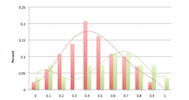
 Mashfiqui Rabbi, Min Hane Aung, Mi Zhang and Tanzeem Choudhury. MyBehavior: Automatic Personalized Health Feedback from User Behavior and Preference using Smartphones. The 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing (Ubicomp 2015) [pdf]
Mashfiqui Rabbi, Min Hane Aung, Mi Zhang and Tanzeem Choudhury. MyBehavior: Automatic Personalized Health Feedback from User Behavior and Preference using Smartphones. The 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing (Ubicomp 2015) [pdf]
-
11.
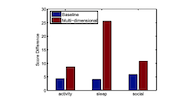
 Mashfiqui Rabbi, Angela Pfammatter, Mi Zhang, Bonnie Spring, and Tanzeem Choudhury. Automated Personalized Feedback for Physical Activity and Dietary Behavior Change With Mobile Phones: A Randomized Controlled Trial on Adults. JMIR mHealth uHealth 2015;3(2):e42 [Impact factor 4.7] [pdf]
Mashfiqui Rabbi, Angela Pfammatter, Mi Zhang, Bonnie Spring, and Tanzeem Choudhury. Automated Personalized Feedback for Physical Activity and Dietary Behavior Change With Mobile Phones: A Randomized Controlled Trial on Adults. JMIR mHealth uHealth 2015;3(2):e42 [Impact factor 4.7] [pdf]
-
10.
 Phil Adams, Mashfiqui Rabbi, Tauhidur Rahman, Mark Matthews, Amy Voida, Geri Gay, Tanzeem Choudhury, and, Stephen Voida. Towards Personal Stress Informatics: Comparing Minimally Invasive Techniques for Measuring Daily Stress in the Wild. International Conference on Pervasive Computing Technologies for Healthcare, 2014 [pdf]
Phil Adams, Mashfiqui Rabbi, Tauhidur Rahman, Mark Matthews, Amy Voida, Geri Gay, Tanzeem Choudhury, and, Stephen Voida. Towards Personal Stress Informatics: Comparing Minimally Invasive Techniques for Measuring Daily Stress in the Wild. International Conference on Pervasive Computing Technologies for Healthcare, 2014 [pdf]
-
9.
 Nicholas D. Lane, Mu Lin, Mashfiqui Rabbi, Xiaochao Yang, Hong Lu, Giuseppe Cardone, Shahid Ali, Ethan Berke, Andrew T. Campbell, Tanzeem Choudhury Bewell: Sensing sleep, physical activities and social interactions to promote wellbeing. Mobile Networks and Applications 19, no. 3 (2014): 345-359 [pdf]
Nicholas D. Lane, Mu Lin, Mashfiqui Rabbi, Xiaochao Yang, Hong Lu, Giuseppe Cardone, Shahid Ali, Ethan Berke, Andrew T. Campbell, Tanzeem Choudhury Bewell: Sensing sleep, physical activities and social interactions to promote wellbeing. Mobile Networks and Applications 19, no. 3 (2014): 345-359 [pdf]
-
8.
 Mu Lin, Nicholas Lane, Mashfiqui Rabbi, Xiaochao Yang, Hong Lu, Giuseppe Cardone, Shahid Ali, Afsaneh Doryab, Ethan Berke, Andrew Campbell, and Tanzeem Choudhury. BeWell+: Multi-dimensional Wellbeing Monitoring with Community-guided User Feedback and Energy Optimization Appears in the Proceedings of Wireless Health 2012, October 2012 [pdf]
Mu Lin, Nicholas Lane, Mashfiqui Rabbi, Xiaochao Yang, Hong Lu, Giuseppe Cardone, Shahid Ali, Afsaneh Doryab, Ethan Berke, Andrew Campbell, and Tanzeem Choudhury. BeWell+: Multi-dimensional Wellbeing Monitoring with Community-guided User Feedback and Energy Optimization Appears in the Proceedings of Wireless Health 2012, October 2012 [pdf]
-
7.
 Hong Lu, Mashfiqui Rabbi, Gokul Chittaranjan, Denise Frauendorfer, Marianne Schmidt, Andrew Campbell, Daneil Gatica-Perez, and Tanzeem Choudhury. StressSense: Detecting Stress in Unconstrained Acoustic Environments using Smartphones. Appears in the Proceedings of Ubicomp 2012, September 2012 [pdf]
Hong Lu, Mashfiqui Rabbi, Gokul Chittaranjan, Denise Frauendorfer, Marianne Schmidt, Andrew Campbell, Daneil Gatica-Perez, and Tanzeem Choudhury. StressSense: Detecting Stress in Unconstrained Acoustic Environments using Smartphones. Appears in the Proceedings of Ubicomp 2012, September 2012 [pdf]
-
6.
 Mashfiqui Rabbi, Shahid Ali, Tanzeem Choudhury, and Ethan Berke. Passive and In-situ Assessment of Mental and Physical Well-being using Mobile Sensors. To appear in the Proceedings of Ubicomp 2011, September 2011. Beijing, China. [pdf]
Mashfiqui Rabbi, Shahid Ali, Tanzeem Choudhury, and Ethan Berke. Passive and In-situ Assessment of Mental and Physical Well-being using Mobile Sensors. To appear in the Proceedings of Ubicomp 2011, September 2011. Beijing, China. [pdf]
-
5.
 Ethan Berke, Tanzeem Choudhury, Shahid Ali, and Mashfiqui Rabbi. Objective Sensing of Activity and Sociability: Mobile Sensing in the Community. Appears in the Annals of Family Medicine, Volume 9, Issue 4, Pages 344-350, July 2011. [pdf] [commentary]
Ethan Berke, Tanzeem Choudhury, Shahid Ali, and Mashfiqui Rabbi. Objective Sensing of Activity and Sociability: Mobile Sensing in the Community. Appears in the Annals of Family Medicine, Volume 9, Issue 4, Pages 344-350, July 2011. [pdf] [commentary]
-
4.
 Nicholas D. Lane, Mashfiqui Rabbi, Mu Lin, Xiaochao Yang, Afsaneh Doryab, Hong Lu, Shahid Ali, Tanzeem Choudhury, Andrew Campbell, and Ethan Berke, BeWell: A Smartphone Application to Monitor, Model and Promote Wellbeing, Pervasive Health 2011-- 5th International ICST Conference on Pervasive Computing Technologies for Healthcare, Dublin, 23-26 May 2011 [pdf]
Nicholas D. Lane, Mashfiqui Rabbi, Mu Lin, Xiaochao Yang, Afsaneh Doryab, Hong Lu, Shahid Ali, Tanzeem Choudhury, Andrew Campbell, and Ethan Berke, BeWell: A Smartphone Application to Monitor, Model and Promote Wellbeing, Pervasive Health 2011-- 5th International ICST Conference on Pervasive Computing Technologies for Healthcare, Dublin, 23-26 May 2011 [pdf]
-
3.
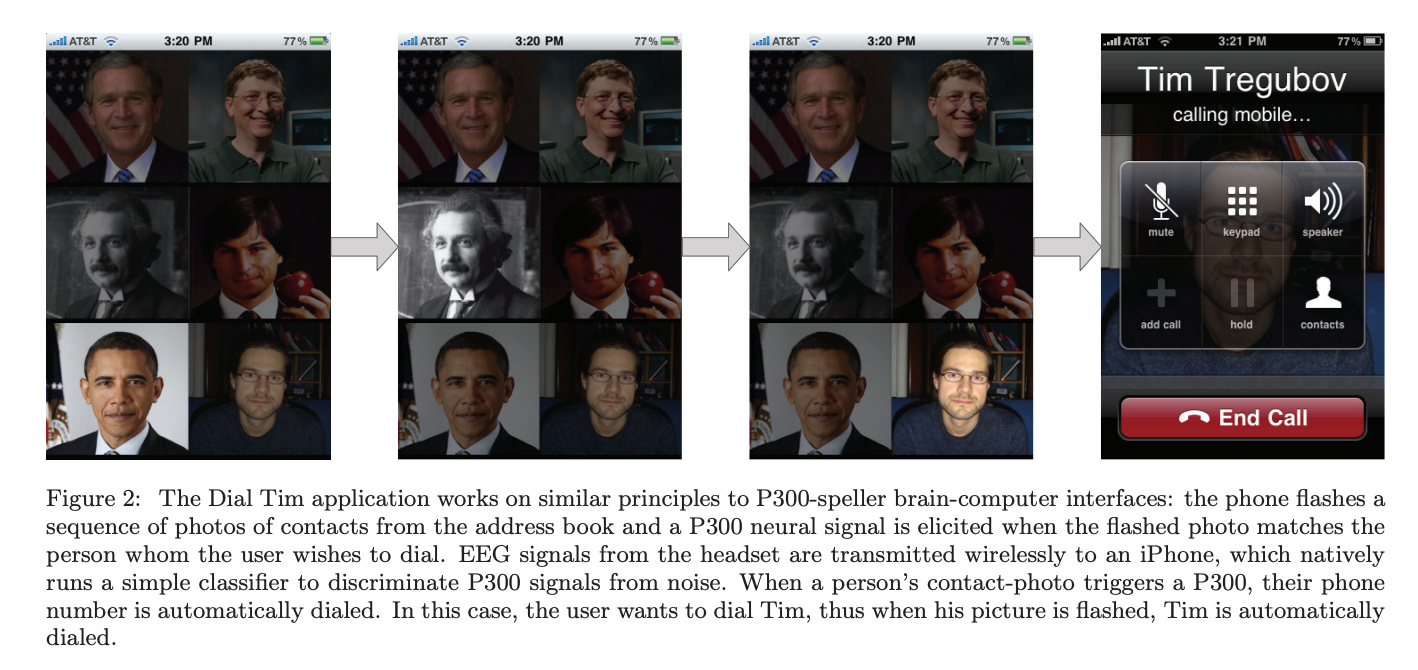
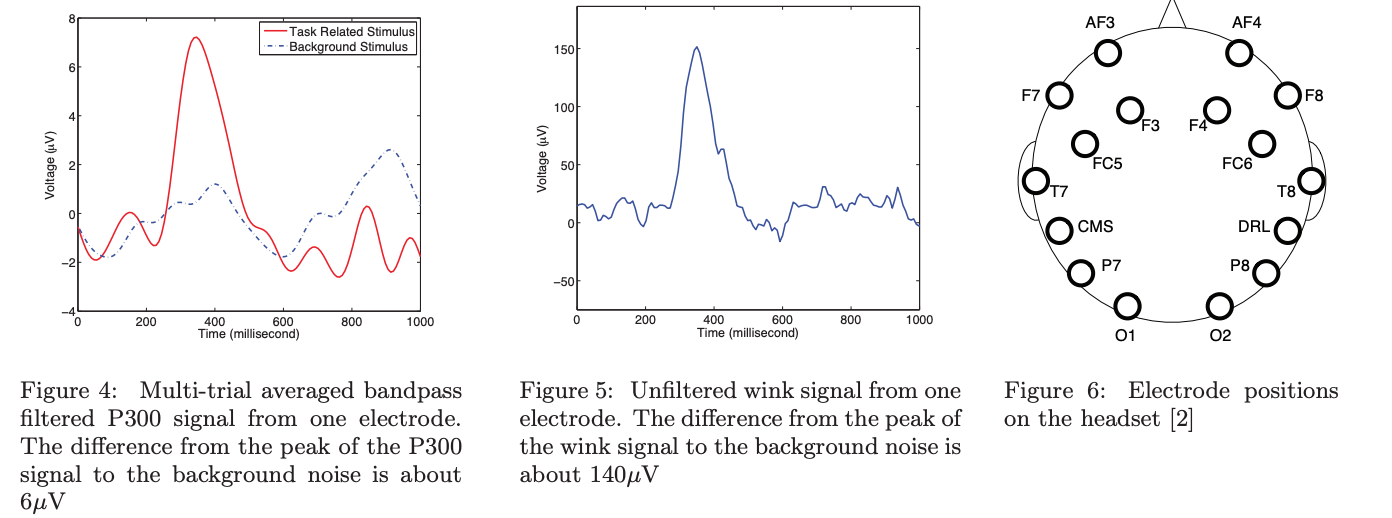
 Andrew T. Campbell, Tanzeem Choudhury, Shaohan Hu, Hong Lu, Matthew Mukerjee, Mashfiqui Rabbi, and Rajeev Raizada. NeuroPhone: Brain-Mobile Phone Interface using a Wireless EEG Headset. Appears in the Proceedings of MobiHeld 2010 [pdf]
Andrew T. Campbell, Tanzeem Choudhury, Shaohan Hu, Hong Lu, Matthew Mukerjee, Mashfiqui Rabbi, and Rajeev Raizada. NeuroPhone: Brain-Mobile Phone Interface using a Wireless EEG Headset. Appears in the Proceedings of MobiHeld 2010 [pdf]
-
2.
 M Jawaherul Alam, Md Abul Hassan Samee, Mashfiqui Rabbi, and Md Saidur Rahman. Minimum-Layer Upward Drawings of Trees. J. Graph Algorithms and Applications 14, no. 2 (2010): 245-267. [pdf]
M Jawaherul Alam, Md Abul Hassan Samee, Mashfiqui Rabbi, and Md Saidur Rahman. Minimum-Layer Upward Drawings of Trees. J. Graph Algorithms and Applications 14, no. 2 (2010): 245-267. [pdf]
-
1.
 M Jawaherul Alam, Mashfiqui Rabbi, and Md Saidur Rahman. Upright Drawings of Planar Graphs on Three Layers. Journal of Applied Mathematics and Informatics, 28(56): 1347-1358, 2010 [pdf]
M Jawaherul Alam, Mashfiqui Rabbi, and Md Saidur Rahman. Upright Drawings of Planar Graphs on Three Layers. Journal of Applied Mathematics and Informatics, 28(56): 1347-1358, 2010 [pdf]
Lightly reviewed posters and workshop papers
-
6.
 Mashfiqui Rabbi, Meredith Philyaw-Kotov, Jinseok Lee, Anthony Mansour, Laura Dent, Xiaolei Wang, Rebecca Cunningham et al. SARA: a mobile app to engage users in health data collection In Proceedings of the 2017 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2017 ACM International Symposium on Wearable Computers, pp. 781-789. ACM, 2017. [pdf]
Mashfiqui Rabbi, Meredith Philyaw-Kotov, Jinseok Lee, Anthony Mansour, Laura Dent, Xiaolei Wang, Rebecca Cunningham et al. SARA: a mobile app to engage users in health data collection In Proceedings of the 2017 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2017 ACM International Symposium on Wearable Computers, pp. 781-789. ACM, 2017. [pdf]
-
5.
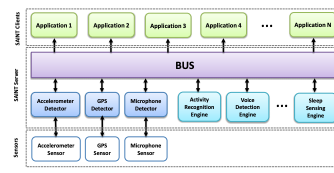 Mashfiqui Rabbi, Thiago Caetano, Jean Costa, Saeed Abdullah, Mi Zhang, and Tanzeem Choudhury. SAINT: A Scalable Sensing and Inference Toolkit. Hotmobile 2015 poster [pdf]
Mashfiqui Rabbi, Thiago Caetano, Jean Costa, Saeed Abdullah, Mi Zhang, and Tanzeem Choudhury. SAINT: A Scalable Sensing and Inference Toolkit. Hotmobile 2015 poster [pdf]
-
4.
 Mashfiqui Rabbi, Syed Ishtiaque Ahmed. Sensing stress network for social coping CSCW Interactive Poster Session, 2014 [pdf | poster]
Mashfiqui Rabbi, Syed Ishtiaque Ahmed. Sensing stress network for social coping CSCW Interactive Poster Session, 2014 [pdf | poster]
-
3.
 Steven Voida, Mark Matthews, Saeed Abdullah, Mengxi C. Chi, Mattew Green, W. J. Jang, D. Hu, Jon Weinrich, P. Patil, Mashfiqui Rabbi, et al. Moodrhythm: tracking and supporting daily rhythms.In Proceedings of the 2013 ACM conference on Pervasive and ubiquitous computing adjunct publication, pages 67-70. ACM, 2013 [pdf]
Steven Voida, Mark Matthews, Saeed Abdullah, Mengxi C. Chi, Mattew Green, W. J. Jang, D. Hu, Jon Weinrich, P. Patil, Mashfiqui Rabbi, et al. Moodrhythm: tracking and supporting daily rhythms.In Proceedings of the 2013 ACM conference on Pervasive and ubiquitous computing adjunct publication, pages 67-70. ACM, 2013 [pdf]
-
2.
 Stephen Voida, Tanzeem Choudhury, Geri Gay, Mark Matthews, Phil Adams, Mashfiqui Rabbi, JP Pollak, Mengxi Chi, Matthew Green, Andrew Campbell, Nic Lane, and Hong Lu. Personal Informatics Can Be Stressful: Collecting, Reflecting, and Embedding Stress Data in Personal Informatics. To Appear in the Proceeding of Personal Informatics Workshop, CHI. [pdf]
Stephen Voida, Tanzeem Choudhury, Geri Gay, Mark Matthews, Phil Adams, Mashfiqui Rabbi, JP Pollak, Mengxi Chi, Matthew Green, Andrew Campbell, Nic Lane, and Hong Lu. Personal Informatics Can Be Stressful: Collecting, Reflecting, and Embedding Stress Data in Personal Informatics. To Appear in the Proceeding of Personal Informatics Workshop, CHI. [pdf]
-
1.
 Mashfiqui Rabbi, Chien wen Yuan, and Kirsikka Kaipaien. An exploratory study to identify opportune moments in everyday life to promote healthy eating.Poster in ISBNPA, 2013 [pdf]
Mashfiqui Rabbi, Chien wen Yuan, and Kirsikka Kaipaien. An exploratory study to identify opportune moments in everyday life to promote healthy eating.Poster in ISBNPA, 2013 [pdf]
Ph.D. Thesis
-
●
 Mashfiqui Rabbi, Automated Mobile Systems For Personalized Health Feedback Cornell University, 2016
Mashfiqui Rabbi, Automated Mobile Systems For Personalized Health Feedback Cornell University, 2016